Introduction
Trypanosomosis is a significant parasitic disease affecting both domestic animals and humans, particularly in tropical and subtropical regions. It is caused by protozoan parasites of the genus Trypanosoma, which are transmitted by arthropod vectors. The disease leads to severe economic losses in livestock production due to morbidity, mortality, and decreased productivity. Human African trypanosomiasis (HAT), also known as sleeping sickness, and animal trypanosomosis, commonly called nagana in cattle, are of major concern. This document provides a comprehensive overview of the disease, including transmission, pathogenesis, clinical signs, diagnosis, treatment, and control strategies.
Transmission of Trypanosomosis
Trypanosomes are transmitted between hosts through two primary mechanisms:
1. Cyclical Transmission
This mode occurs through biological vectors where the parasites undergo development and multiplication. It is further classified into:
- Salivarian Trypanosomes: Transmitted by tsetse flies (Glossina species) through the anterior station development. This includes Trypanosoma brucei, T. congolense, and T. vivax, which cause disease in cattle, horses, and other domestic animals.
- Stercorarian Trypanosomes: These develop in the hindgut of the vector and are transmitted via feces contamination, as seen in T. cruzi, which causes Chagas disease in humans and dogs, transmitted by triatomine bugs.
2. Non-Cyclical Transmission
In this mechanical transmission, trypanosomes are transferred directly from one host to another by biting insects without undergoing development in the vector. Examples include:
- Trypanosoma evansi (causing Surra in camels and horses) is transmitted by horseflies (Tabanus spp.) and stable flies (Stomoxys spp.).
- In Latin America, vampire bats (Desmodus rotundus) act as reservoirs and vectors of T. evansi.
- Venereal transmission occurs in T. equiperdum, responsible for dourine in equines.
Pathogenesis and Clinical Manifestations
The severity of trypanosomosis depends on the species, host susceptibility, and immune response. The pathogenesis involves:
1. Immune Evasion and Chronic Infection
Trypanosomes evade host immunity through antigenic variation, where they continuously change their surface glycoproteins. This leads to persistent infection and immune exhaustion.
2. Hemolysis and Anemia
- Destruction of red blood cells occurs due to direct parasitic action and immune-mediated lysis.
- Anemia is exacerbated by splenic sequestration and phagocytosis of erythrocytes.
3. Inflammatory and Organ Damage
- The spleen and lymph nodes become enlarged due to immune activation.
- Myocardial degeneration and heart failure are common in chronic cases.
- In T. brucei infections, the central nervous system (CNS) is affected, leading to meningoencephalitis.
Clinical Signs in Domestic Animals
- Cattle (Nagana): Progressive weight loss, anaemia, fever, lethargy, edema, and reduced milk production.
- Horses and Camels (Surra & Dourine): Oedema, fever, ataxia, genital swelling, and neurological signs in dourine.
- Pigs: T. simiae causes hyperacute infections with high mortality.
- Dogs & Cats: Fever, lymphadenopathy, myocarditis, corneal opacity, and neurological disorders.
Epidemiology
Trypanosomosis is endemic in regions where suitable vectors thrive. Key epidemiological factors include:
- Sub-Saharan Africa: Endemic due to tsetse fly distribution; wildlife reservoirs contribute to transmission.
- Asia & South America: Mechanical transmission of T. evansi by biting flies and vampire bats.
- Trypanotolerant Breeds: Some cattle breeds, such as N’Dama and West African Shorthorn, show natural resistance.
Diagnosis
Accurate diagnosis is essential for effective control. Common diagnostic techniques include:
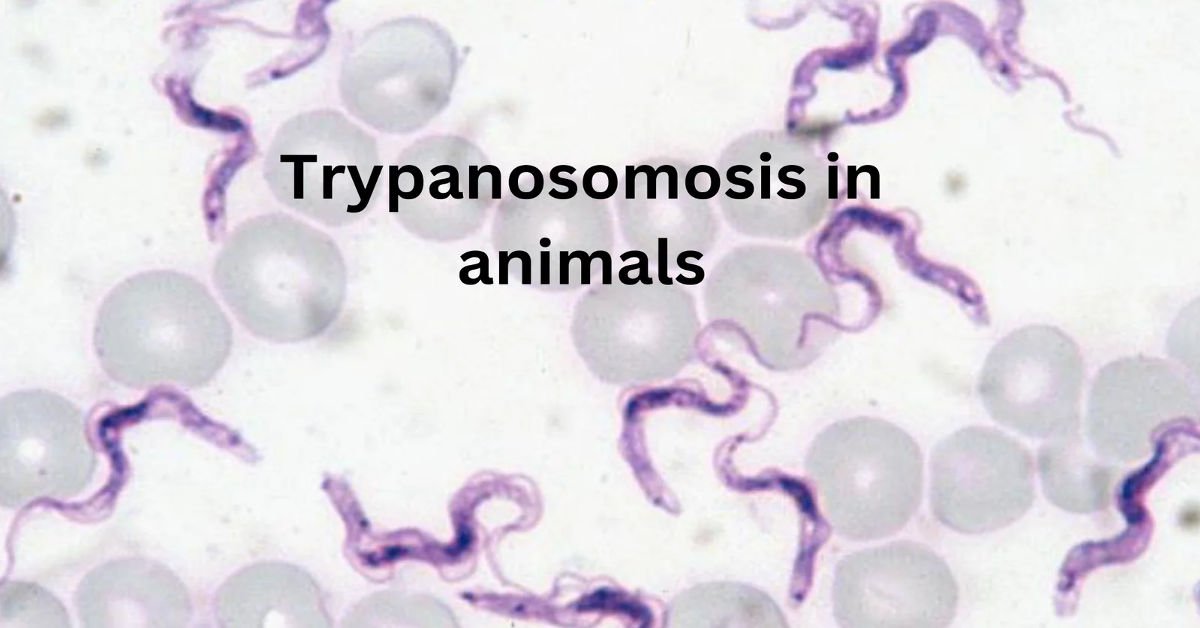
1. Direct Microscopy
- Giemsa-stained blood smears to detect motile trypanosomes.
- Buffy coat concentration using microhematocrit centrifugation.
2. Serological Tests
- ELISA and complement fixation tests for antigen and antibody detection.
3. Molecular Techniques
- PCR and Loop-Mediated Isothermal Amplification (LAMP) for species-specific identification.
Treatment and Chemotherapy
Treatment options vary based on species and drug availability:
- Diminazene aceturate (Berenil): Effective against T. congolense and T. brucei.
- Homidium salts (Ethidium & Novidium): Used in cattle, but resistance is a concern.
- Suramin & Quinapyramine: Used for T. evansi in camels and horses.
- Melarsoprol: Used for CNS involvement but is highly toxic.
- Isometamidium chloride: Has prophylactic properties in cattle.
Drug Resistance
Emerging resistance to trypanocidal drugs is a major concern. Resistance mechanisms include reduced drug uptake, increased efflux, and metabolic detoxification. Combination therapy and rotational use of drugs are recommended strategies.
Control and Prevention Strategies
Effective control of trypanosomosis requires an integrated approach:
1. Vector Control
- Tsetse fly eradication: Using insecticide-treated targets, aerial spraying, and sterile insect technique.
- Use of Pour-on Insecticides: Controls biting flies responsible for mechanical transmission.
2. Chemoprophylaxis
- Regular prophylactic treatment in endemic areas prevents severe infections.
3. Breeding of Trypanotolerant Livestock
- Use of resistant breeds such as N’Dama cattle in Africa.
4. Vaccination Research
- No commercial vaccines exist due to antigenic variation, but research is ongoing to develop alternative strategies such as recombinant vaccines and immune-modulatory approaches.
Modern research about Trypanosomosis in animals
Current studies on trypanosomosis in animals, caused by Trypanosoma parasites, focus on innovative diagnostics, treatments, and prevention. Spread mainly by tsetse flies, this disease impacts livestock across Africa, Asia, and Latin America, leading to substantial economic losses. A 2023 study highlights molecular tools like qPCR for detecting parasite DNA and loop-mediated isothermal amplification (LAMP) for field diagnostics, though antigen-based tests struggle with sensitivity. Research into trypanotolerant breeds, such as Djallonké sheep, identifies genetic traits for breeding resistant animals. Drug treatments like isometamidium face resistance issues, driving efforts to discover novel compounds. Vector control strategies, including pheromone traps and drone-based insecticide delivery, reduce tsetse populations effectively. The One Health framework emphasizes managing trypanosomosis at the livestock-wildlife interface to limit zoonotic risks. Vaccine development remains elusive due to the parasite’s antigenic variability, but immunotherapy research shows potential. Geospatial tools now guide targeted interventions by mapping high-risk areas. These efforts aim to enhance animal welfare and secure agricultural economies, addressing both local and global challenges posed by this debilitating disease.
Public Health Concerns of Trypanosomosis in Animals
Trypanosomosis, transmitted mainly by tsetse flies (Glossina spp.), affects livestock and wildlife across sub-Saharan Africa, posing significant public health and economic challenges. Its zoonotic potential and impact on food security make it a critical concern.
AAT is a major constraint to livestock production, infecting cattle, sheep, goats, pigs, and other animals. Infected animals suffer from fever, anemia, weight loss, and reduced fertility, leading to decreased milk and meat production. The disease causes an estimated annual economic loss of $4.5 billion in sub-Saharan Africa due to reduced agricultural productivity and increased treatment costs. This impacts food security, as communities reliant on livestock face malnutrition risks when herds are decimated. In regions like Uganda and Ghana, prevalence rates in cattle can reach 22.15% under DNA diagnostic methods, highlighting the disease’s widespread impact.
The public health concern extends beyond animals due to the zoonotic nature of certain Trypanosoma species. T. brucei rhodesiense, responsible for acute human African trypanosomiasis (HAT) or sleeping sickness, is primarily hosted by domestic cattle and wildlife, serving as reservoirs. T. brucei gambiense, causing chronic HAT, can also infect animals like pigs and dogs, complicating elimination efforts. A 2024 review in Nigeria noted a 3.6% HAT prevalence, underscoring ongoing challenges. These cases, though rare, raise alarms about emerging zoonotic threats, particularly in areas with high animal trypanosome prevalence.
Human activities exacerbate the risk. Increased land use for grazing and settlement near wildlife reserves heightens wildlife-livestock-human interactions, facilitating pathogen spillover. Tsetse-rich game parks pose transmission risks to nearby communities. Ineffective vector control and drug resistance further complicate management. Trypanocidal drugs, widely used for AAT, face resistance due to substandard products and overuse, reducing treatment efficacy.
A One Health approach is essential for control. Integrated strategies, like those of the Animal and Human Health for the Environment and Development (AHEAD) program, combine vector control, improved diagnostics, and community education to mitigate risks. Insecticide-treated nets and traps reduce tsetse populations, while selecting trypanotolerant breeds like N’Dama cattle lessens disease impact. Enhanced surveillance and molecular diagnostics, such as PCR, improve detection of trypanosomes in animals and humans, aiding targeted interventions.
In conclusion, trypanosomosis in animals is a multifaceted public health issue, threatening food security and human health through zoonotic transmission. Addressing it requires coordinated efforts in vector control, diagnostics, and sustainable livestock management to safeguard communities and economies in affected regions.
Conclusion
Trypanosomosis remains a major constraint to livestock production and human health in endemic regions. A multifaceted approach, including vector control, improved diagnostics, rational drug use, and research on vaccine development, is crucial to managing the disease effectively. Future efforts should focus on sustainable strategies, including genetic improvement of livestock and enhanced surveillance programs.
FAQ’S
What is trypanosomosis?
Trypanosomosis is caused by protozoan parasites of the genus Trypanosoma. It affects both animals and humans, leading to significant morbidity and mortality, particularly in tropical and subtropical regions.
2. How is trypanosomosis transmitted?
Trypanosomosis is primarily transmitted through the bites of infected arthropod vectors, such as tsetse flies, tabanids, and Stomoxys. In some cases, transmission can occur mechanically via biting insects or through direct contact, as in the case of Trypanosoma equiperdum, which causes a venereal disease in horses.
3. What are the main species of trypanosomes that affect animals?
The most significant species include:
- Salivaria Group: Trypanosoma brucei, T. congolense, and T. vivax (transmitted by tsetse flies).
- Stercoraria Group: Trypanosoma cruzi (causes Chagas disease in humans) and T. evansi (transmitted mechanically by biting flies and vampire bats).
4. What are the clinical signs of trypanosomosis in animals?
Clinical signs vary depending on the species of trypanosome and the host. Common signs include:
- Anemia: A hallmark of the disease.
- Lymphadenopathy: Enlarged lymph nodes.
- Emaciation: Progressive weight loss.
- Fever: Intermittent or persistent.
- Neurological signs: In advanced cases, especially with T. brucei infections.
- Edema: Swelling of limbs, genitalia, or ventral abdomen.
5. How is trypanosomosis diagnosed?
Diagnosis is based on:
- Microscopic examination: Detection of trypanosomes in blood smears.
- Centrifugation techniques: Concentration of parasites in microhaematocrit tubes.
- Serological tests: ELISA or complement fixation tests to detect antibodies or antigens.