Introduction
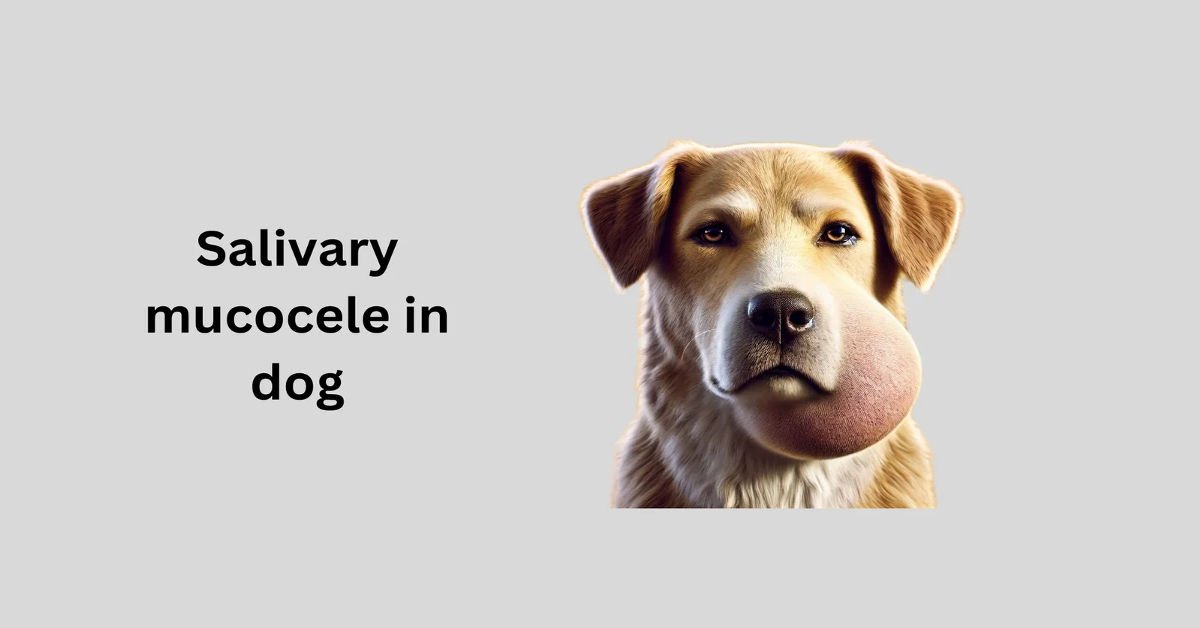
Salivary mucocele in dogs, also known as sialocele, is a condition where saliva accumulates in tissues due to damage to a salivary gland or duct. Unlike true cysts, mucoceles lack an epithelial lining and are surrounded by granulation tissue. Causes include trauma, sialoliths (salivary stones), and foreign bodies.
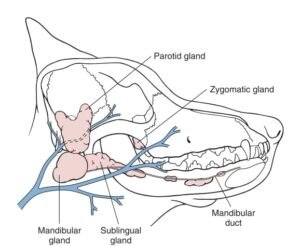
Salivary glands in dogs
Types of Salivary Mucocele
The classification of salivary mucoceles is based on their location:
| Type | Location |
|---|---|
| Cervical Mucocele | Intermandibular or upper cervical region |
| Sublingual Mucocele (Ranula) | Beneath the tongue near mandibular and sublingual ducts |
| Pharyngeal Mucocele | Near the pharynx, may cause respiratory distress |
| Zygomatic Mucocele | Ventral to the eye, affecting vision and facial swelling |
| Complex Mucocele | Involves multiple locations simultaneously |
Pathophysiology
Damage to the salivary gland or duct causes saliva leakage into surrounding tissues, leading to inflammation. The sublingual gland is most commonly affected. This condition frequently occurs in dog breeds like Poodles, German Shepherds, Dachshunds, and Australian Silky Terriers.
Types of salivary mucocele
| Mucocele Type | Symptoms |
| Cervical Mucocele | Painless, fluctuant swelling |
| Ranula | Oral bleeding, difficulty eating |
| Pharyngeal Mucocele | Respiratory distress, dysphagia |
| Zygomatic Mucocele | Facial swelling, enophthalmos, strabismus |
Physical Examination
Most mucoceles are soft, non-painful, and fluctuant. Palpation can determine the affected side. Blood-tinged saliva is common in ranulas. Pharyngeal mucoceles may obstruct airways, requiring emergency intervention.
Diagnostic Imaging and Laboratory Findings
| Diagnostic Tool | Use |
| Radiographs | Rarely useful unless sialoliths or neoplasia are suspected |
| Sialography | Confirms the affected gland but is rarely needed |
| Ultrasound/CT | Helpful in complex or zygomatic mucoceles |
| Cytology | Fine-needle aspiration shows mucoid fluid; PAS stain confirms saliva |
Differential Diagnoses
When evaluating a dog for a suspected salivary mucocele, veterinarians consider other conditions that may present with similar symptoms, such as swellings in the neck, jaw, mouth, or near the eye. The following are key differential diagnoses, categorized by clinical presentation:
- Abscess:
- Description: A localized infection with pus accumulation, often due to trauma, foreign bodies, or dental disease.
- Distinguishing Features:
- Painful, warm, and possibly red swelling, unlike the typically non-painful mucocele.
- Fine-needle aspiration yields pus (bacteria, white blood cells) rather than clear or mucoid saliva.
- Systemic signs (e.g., fever, lethargy) are more common.
- Diagnostics: Aspiration, cytology, culture, and imaging to rule out foreign bodies.
- Neoplasia (Tumor):
- Description: Benign or malignant tumors of the salivary gland (e.g., adenoma, adenocarcinoma) or nearby tissues (e.g., lymphoma, mast cell tumor).
- Distinguishing Features:
- Firm, irregular, or fixed masses rather than soft, fluctuant mucoceles.
- May cause systemic signs (e.g., weight loss) or local invasion (e.g., bone erosion).
- Aspiration may show abnormal cells; biopsy is often needed.
- Diagnostics: Imaging (ultrasound, CT), cytology, or biopsy to confirm.
- Cyst:
- Description: Fluid-filled structures, such as branchial or thyroglossal cysts, unrelated to salivary glands.
- Distinguishing Features:
- Location may differ (e.g., midline neck for thyroglossal cysts).
- Diagnostics: Imaging and histopathology to differentiate.
- Hematoma/Seroma:
- Description: Blood (hematoma) or serous fluid (seroma) accumulation due to trauma or surgery.
- Diagnostics: Aspiration and history review.
- Lymphadenopathy:
- Description: Enlarged lymph nodes due to infection, inflammation, or neoplasia (e.g., lymphoma).
- Distinguishing Features:
- Firm, nodular swellings, often in multiple locations (e.g., submandibular lymph nodes).
- Aspiration shows lymphoid cells or pus, not saliva.
- Systemic signs may be present (e.g., fever, weight loss).
- Diagnostics: Cytology, biopsy, or imaging.
- Soft Tissue Swelling (Edema):
- Description: Fluid accumulation due to inflammation, allergic reactions, or trauma.
- Distinguishing Features:
- Diffuse, pitting swelling rather than a discrete, fluctuant mass.
- Aspiration may yield minimal fluid, not saliva.
- Often resolves with anti-inflammatories or time.
- Diagnostics: History, physical exam, and response to treatment.
- Salivary Gland Inflammation (Sialadenitis):
- Distinguishing Features:
- Painful, firm gland rather than a soft mucocele.
- Aspiration may show inflammatory cells or pus.
- May precede mucocele formation if untreated.
- Diagnostics: Cytology, culture, and imaging.
- Distinguishing Features:
- Foreign Body Reaction:
- Description: Tissue reaction to embedded objects (e.g., plant material, bone fragments).
- Distinguishing Features:
- Painful, possibly draining swelling with a history of chewing or trauma.
- Aspiration may reveal pus or debris, not saliva.
- Diagnostics: Imaging, surgical exploration.
| Condition | Differentiating Factor |
| Sialoadenitis | Inflammation of the salivary gland |
| Sialadenosis | Non-inflammatory gland swelling |
| Neoplasia | Tumorous growth |
| Abscess | Infection-related swelling |
| Foreign Body | Presence of an external object |
Treatment Options
A salivary mucocele (sialocele) in dogs occurs when saliva leaks from a damaged salivary gland or duct, forming a fluid-filled swelling in surrounding tissues. The prognosis is generally good to excellent with appropriate treatment, and below is a detailed, plagiarism-free overview of the prognosis and treatment options, tailored to your request.
Prognosis:
- With Surgical Treatment:
- Surgical removal of the affected salivary gland and duct (sialoadenectomy) is the most effective treatment, offering an excellent prognosis with recurrence rates below 5% when the correct gland is removed.
- Most dogs recover fully within 10–14 days, with minimal complications (e.g., infection, seroma) if post-operative care is followed.
- Early intervention enhances outcomes and prevents chronic issues.
- Without Treatment:
- Untreated mucoceles rarely resolve spontaneously and may enlarge, causing discomfort, difficulty eating, breathing issues (especially pharyngeal mucoceles), or secondary infections.
- Chronic cases can lead to tissue scarring or damage, complicating future treatment and worsening prognosis.
- With Conservative Management:
- Non-surgical approaches, like aspiration or medication, often result in recurrence, offering a poorer long-term prognosis compared to surgery.
- These methods may provide temporary relief but do not address the underlying gland dysfunction.
- Factors Affecting Prognosis:
- Type/Location: Cervical (neck/jaw) and ranula (sublingual) mucoceles are common and have high surgical success rates. Zygomatic (near the eye) or pharyngeal (throat) mucoceles are more complex but still treatable with good outcomes.
- Cause: Trauma, tumors, or obstructions (e.g., foreign bodies) must be addressed to optimize recovery.
- Timeliness: Prompt treatment reduces complications and improves success.
- Dog’s Health: Concurrent conditions (e.g., infections, clotting issues) may slightly lower the prognosis.
- Recurrence:
- Recurrence is rare post-surgery but can occur if the wrong gland is removed or multiple glands are involved.
- Diagnostic imaging (e.g., ultrasound, CT, or sialography) helps identify the affected gland, minimizing this risk.
- Recovery:
- Post-surgical recovery is typically swift, with dogs returning to normal within 1–2 weeks.
- Mild swelling or fluid buildup at the site may occur but usually resolves naturally or with minor intervention.
- Owners should monitor for signs of complications (e.g., excessive swelling, discharge) and follow veterinary care instructions.
Treatment Options:
- Surgical Removal (Sialoadenectomy):
- Description: The affected salivary gland and duct are surgically removed to prevent further saliva leakage. Common for cervical, sublingual, pharyngeal, or zygomatic mucoceles.
- Pros:
- Most effective, with a high cure rate and low recurrence risk.
- Resolves symptoms permanently in most cases.
- Cons:
- Requires general anesthesia, which carries minor risks.
- Costs vary ($500–$3,000, depending on diagnostics, location, and complexity).
- Potential complications include seroma, infection, or nerve damage (rare).
- Procedure:
- Pre-surgical imaging (e.g., ultrasound, CT) may be used to identify the gland.
- The gland is excised, and a drain may be placed to prevent fluid buildup.
- Post-op care includes pain management, antibiotics (if needed), and activity restriction.
- Best For: Most cases, especially when the mucocele is large, recurrent, or causing significant symptoms.
- Aspiration and Drainage:
- Description: A needle is used to drain the accumulated saliva from the mucocele, sometimes followed by injection of anti-inflammatory or sclerosing agents to reduce swelling.
- Pros:
- Minimally invasive and less expensive than surgery.
- Can provide temporary relief for small mucoceles or as a diagnostic step.
- Cons:
- High recurrence rate, as the underlying gland issue persists.
- Repeated procedures may be needed, increasing costs over time.
- Risk of infection if not performed sterilely.
- Best For: Cases where surgery is not immediately feasible (e.g., financial constraints, poor surgical candidate) or as a temporary measure.
- Medical Management:
- Description: Involves antibiotics (for secondary infections) or anti-inflammatory medications to manage symptoms.
- Pros:
- Non-invasive and low-cost.
- May reduce swelling or discomfort temporarily.
- Cons:
- Does not address the mucocele itself, leading to recurrence.
- Limited to cases with mild symptoms or secondary complications.
- Best For: Dogs with concurrent infections or as supportive care alongside other treatments.
- Marsupialization (for Ranulas):
- Description: For sublingual mucoceles (ranulas), the mucocele is opened, and its lining is sutured to the oral mucosa to create a permanent opening for saliva drainage.
- Pros:
- Less invasive than gland removal in some cases.
- Effective for specific ranula cases.
- Cons:
- Not suitable for all mucocele types.
- Risk of recurrence if the underlying gland continues to leak.
- Best For: Oral ranulas where gland removal is not preferred.
- Observation:
- Description: Monitoring small, asymptomatic mucoceles without immediate intervention.
- Pros:
- Avoids unnecessary procedures for minor cases.
- No cost or risk initially.
- Cons:
- Most mucoceles worsen over time, requiring eventual treatment.
- Risk of complications like infection or growth.
- Best For: Rare cases of small, non-painful mucoceles with no impact on quality of life.
Additional Considerations:
- Diagnostics: Accurate diagnosis is critical. Physical exams, fine-needle aspiration, and imaging (ultrasound, CT, or sialography) help confirm the mucocele and identify the affected gland.
- Breeds: Predisposed breeds (e.g., Poodles, German Shepherds, brachycephalics) may require closer monitoring, but treatment outcomes remain similar.
- Quality of Life: Surgery typically restores normal function, while untreated mucoceles may cause ongoing discomfort or complications.
- Cost: Surgical costs depend on the case complexity and location, while non-surgical options may seem cheaper initially but become costly with recurrences.
Recommendations:
- Consult a veterinarian for a thorough evaluation, including imaging if needed, to confirm the mucocele type and affected gland.
- Surgery is the gold standard for most cases, offering the best chance for a permanent cure.
- If surgery isn’t an option, discuss drainage or medical management with your vet, understanding their temporary nature.
- Monitor your dog for symptoms like swelling, pain, or difficulty eating, and seek prompt care to improve outcomes.
| Treatment | Purpose |
| Emergency aspiration | Needed for pharyngeal mucoceles causing distress |
| Repeated drainage | Ineffective, increases infection risk |
| Sclerosing agents | Rarely used due to complications |
Surgical Management
Surgical excision of the affected gland is the definitive treatment.
Mandibular and Sublingual Salivary Gland Excision
| Step | Procedure |
| Incision | Longitudinal cut from the mandible angle |
| Exposure | Dissect mandibular gland from connective tissue |
| Identification | Locate the sublingual gland and duct |
| Ligation & Excision | Transect duct near the lingual nerve |
| Closure | Use absorbable sutures |
Postoperative Care: NSAIDs, 7-10 days recovery, monitor for seroma.
Parotid Salivary Gland Excision
| Step | Procedure |
| Incision | Curved cut along ear’s ventral border |
| Exposure | Dissect to expose parotid gland |
| Ligation & Excision | Transect parotid duct carefully |
| Closure | Standard suturing techniques |
Postoperative Care: Monitor for facial nerve damage.
Zygomatic Salivary Gland Excision
| Step | Procedure |
| Incision | Small cut over the zygomatic arch |
| Exposure | Dissect through orbicularis oculi muscle |
| Ligation & Excision | Ligate duct, avoid optic nerve |
| Closure | Reposition the zygomatic arch, close in layers |
Postoperative Care: Monitor for ocular complications.
Prognosis
The prognosis is generally favorable to excellent with proper treatment. Outcomes vary based on the mucocele type, cause, and management approach.
Prognosis Overview:
- Surgical Intervention:.
- This approach yields an excellent prognosis, with recurrence rates below 5% when the correct gland is excised.
- Most dogs recover fully within 1–2 weeks, assuming no complications like infection or seroma (fluid buildup) occur, which are rare.
- Untreated Cases:
- Without treatment, mucoceles rarely resolve on their own and may grow, causing pain, swelling, or issues like difficulty swallowing or breathing (particularly with pharyngeal mucoceles).
- Chronic cases risk infections or tissue scarring, which can complicate future treatment and worsen outcomes.
- Non-Surgical Management:
- Draining the mucocele or using medications (e.g., antibiotics for infections) is sometimes tried but often leads to recurrence.
- The prognosis with these methods is less favorable, as they don’t address the root cause.
- Influencing Factors:
- Location and Type: Common mucoceles, like cervical (neck/jaw swelling) or ranulas (under the tongue), respond well to surgery. Zygomatic or pharyngeal mucoceles, though trickier due to their location, still have good outcomes with expert care.
- Cause: Trauma, tumors, or blockages (e.g., foreign objects) must be resolved to optimize prognosis.
- Timing: Early treatment improves success and reduces complications.
- Dog’s Health: Underlying conditions (e.g., immune issues) may slightly lower the prognosis.
- Recurrence Risk:
- Recurrence is uncommon after proper surgery but possible if the wrong gland is removed or multiple glands are affected.
- Advanced imaging (e.g., ultrasound or CT) can help pinpoint the gland, reducing this risk.
- Recovery Expectations:
- Post-surgery, dogs typically resume normal activity within 10–14 days.
- Minor swelling at the surgical site may occur but usually resolves without intervention.
- Owners should watch for signs of trouble, like persistent swelling or eating difficulties, and adhere to care instructions.
Other Notes:
- Breed Factors: Some breeds (e.g., Poodles, German Shepherds) may be more prone, but breed doesn’t significantly alter prognosis.
- Cost Considerations: Surgery costs ($500–$3,000) may affect treatment decisions, but it remains the most reliable option.
- Quality of Life: Treated dogs generally regain full function, while untreated mucoceles may cause ongoing discomfort.
Suggestions:
- Seek a veterinary evaluation, including possible imaging, to confirm the mucocele and plan treatment.
- Surgery offers the best chance for a cure and long-term relief.
- If surgery isn’t feasible, ask your vet about interim options, though these are less effective.
| Factor | Outcome |
| Complete Gland Removal | Excellent prognosis |
| Partial Excision | Risk of recurrence |
| Nerve Damage | Transient hypoglossal dysfunction |
| Seroma Formation | Possible but manageable |
When to Visit a Veterinarian
It is crucial to consult a veterinarian if your dog exhibits any of the following signs:
- Swelling in the neck, mouth, or face
- Difficulty eating or swallowing
- Respiratory distress
- Oral bleeding or excessive drooling
- Persistent discomfort or pain
Early intervention ensures better outcomes and prevents complications.
FAQs
Q1: Can salivary mucocele resolve on its own? Salivary mucoceles typically require surgical removal of the affected gland to prevent recurrence.
Q2: How long is the recovery period after surgery? Most dogs recover within 7-10 days with proper postoperative care.
Q3: Is salivary mucocele painful for dogs? While mucoceles are usually painless, they can cause discomfort if they interfere with eating, breathing, or vision.
Q4: Can salivary mucoceles come back after treatment? Recurrence is rare if the affected gland is completely excised.
Q5: What breeds are most prone to salivary mucoceles? Poodles, German Shepherds, Dachshunds, and Australian Silky Terriers are more commonly affected.
Conclusion
Salivary mucocele is a common but treatable condition in dogs. Diagnosis relies on clinical presentation and cytology. Surgical excision provides a permanent cure, with a high success rate. Early intervention is crucial, especially for cases causing respiratory distress.
It is crucial to consult a veterinarian if your dog exhibits any of the following signs:
- Swelling in the neck, mouth, or face
- Difficulty eating or swallowing
- Respiratory distress
- Oral bleeding or excessive drooling
- Persistent discomfort or pain
Early intervention ensures better outcomes and prevents complications.